65 YEARS OLD FEMALE WITH SYNCOPE
This is an online e log book to discuss our patient's de-identified health data shared after taking his/her/guardians' signed informed consent. This Elog reflects my patient-centered online learning portfolio.
A 65 year old female, housewife, resident of Chinatunalgudam presented to the casualty with loss of consciousness.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic two days ago. Then, after walking for a long time, she had an episode of syncope, associated with sweating,
After gaining consciousness after approximately.
Not associated with palpitations, flushing, chest pain, muscle weakness, slurring of speech, headache.
The patient was brought to the casualty and given medication (glucose saline) and recovered completely.
PAST HISTORY:
4 days ago, patient has history of chest pain (sudden onset , in the centre of chest, squeezing type, non progressive, not radiating ) with shortness of breath following exertion, which was relieved on rest.
She went to an RMP and was given an anti-hypertensive agent. (which she consumed for the first time 3 days ago)
No similar complaints in the past
She is a known case of hypertension since 3days
Not a known case of diabetes mellitus, asthma, tb, cerebrovascular accidents, coronary artery disease .
No blood transfusions .
History of treatment for cellulitis of leg 3 years back.
FAMILY HISTORY:
3 siblings with DM
PERSONAL HISTORY:
Mixed diet , normal appetite
Adequate sleep
Normal bowel and bladder movements
No allergies
Addiction - sutta- 4 cigarettes/ day since 40 years
Alcohol or toddy - 1 glass daily
MENSTRUAL HISTORY:
Age of menopause: 48 years of age
GENERAL EXAMINATION:
The patient is conscious, coherent, and cooperative
Moderately built and moderately nourished
There is no Pallor, icterus, cyanosis, koilonychia, lymphadenopathy.
Pedal edema present till below knee
VITALS:
BP- 120/80mmHg in sitting position with cuff in the right hand at the level of the heart
PR- 67 bpm, normal in rhythm, rate, volume and character. No radioradial / radiofemoral delay
RR- 20cpm
Temp- Afebrile
SYSTEMIC EXAMINATION:
CNS:
Higher Mental Functions
Normal speech and language
Normal memory
No delusions or hallucinations
Cranial nerve examination
I: Intact bilaterally
III, IV, VI: Extraocular movements free and full bilaterally
V: Intact bilaterally
VII: Intact bilaterally
VIII: No nystagmus, intact bilaterally
IX,X: Intact bilaterally
XII: Intact bilaterally
MOTOR SYSTEM
Bulk- normal
Power: normal. Power of:
- Shoulder , Elbow , Wrist , Smalll muscle of hand and hand grip bilaterally
- knee , ankle bilaterally
Muscle tone: normal
Reflexes - Biceps , triceps , knee jerk , ankle jerk bilaterally - +2
Cerebellar signs: Absent
Sensory system examination
Upper limb:
- Crude touch, temperature, fine touch, vibration sensation present bilaterally
- Pain sensation is normal bilaterally
Lower limb:
- Crude touch, temperature, fine touch, vibration sensation present bilaterally
- Pain sensation is normal bilaterally
CVS
S1 S2 heard , no murmur
No thrill
Apical impulse felt
RESPIRATORY
Normal vesicular breath sounds in all areas
No adventitious breath sounds
PER ABDOMEN
Obese abdomen, umbilicus central and everted
Soft , non tender
No hepatomegaly no splenomegaly
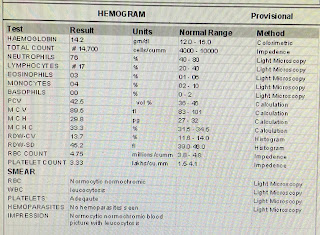
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
?Heat exhaustion
?TIA
?Hypotension
Daily routine
Wake up - 7 am
8 am - breakfast (rice )and tea
Afternoon - lunch ( rice and curry )
Dinner - 9pm rice and curry .
Sleep - 10 pm
SOAP NOTES:
TREATMENT:


















Comments
Post a Comment